Send sunshine prior authorization form pdf via email, link, or fax. You can also download it, export it or print it out.

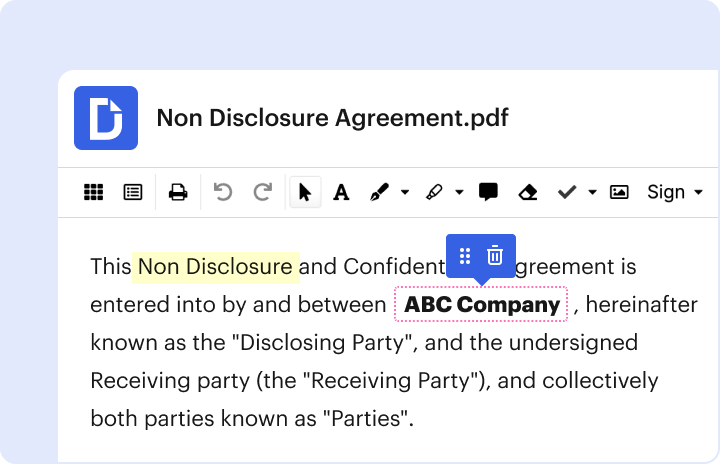
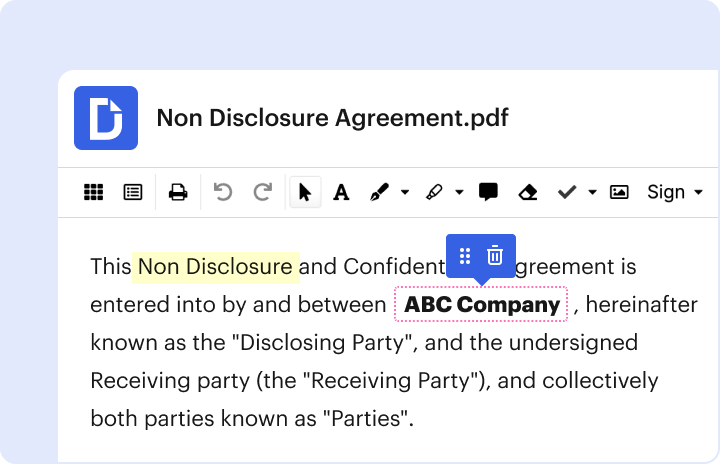
Dochub is the greatest editor for modifying your forms online. Adhere to this simple instruction to redact Sunshine prior authorization form in PDF format online for free:
Try all the benefits of our editor today!
Fill out sunshine prior authorization form onlineWe have answers to the most popular questions from our customers. If you can't find an answer to your question, please contact us.
Is Florida Medicaid the same as Sunshine Health?Sunshine Health is a Florida Medicaid health plan that has been providing services in Florida since 2009.
Does Sunshine Medicaid require referrals for specialists?Remember, you may need a referral from your Primary Care Provider (PCP) or approval from us before you go to an appointment or use a service. Services must be medically necessary (PDF) in order for us to pay for them.
What kind of insurance is sunshine health?Sunshine Health is among the largest comprehensive healthcare plans in Florida. We provide quality healthcare coverage with expanded benefits to individuals and families to help them get well and stay well through through our Medicaid, Long Term Care and specialty plans.
Is Sunshine State Health Medicaid?Sunshine Health enrolls members who are eligible for Medicare and Medicaid. Medicaid includes Full-Benefit Dual Eligible, Qualified Medicare Beneficiary Plus (QMB+) and Specified Low-Income Medicare Beneficiary Plus (SLMB+). Currently, this plan has 2,679 members in 20 counties.
Who bought Sunshine Health?Centene Corporation finalized its acquisition of WellCare Health Plans, Inc. on January 23, 2020. Centene is the parent company of Sunshine Health; WellCare is the parent company of WellCare of Florida and Staywell Health Plan.
sunshine prior authorization form pdf sunshine medicaid prior authorization form (pdf) sunshine health prior authorization fax form sunshine authorization lookup tool sunshine health outpatient behavioral health prior authorization form sunshine health authorization phone number sunshine health forms sunshine health ltc authorization form
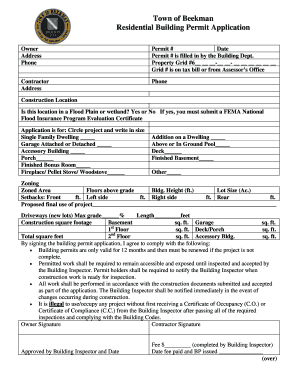
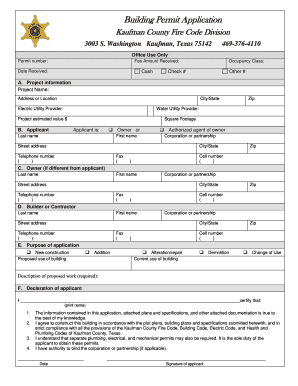
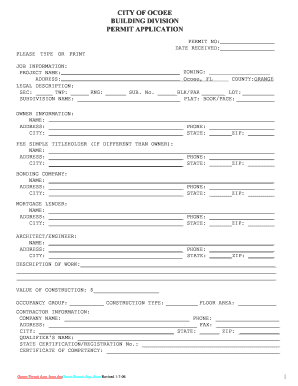
Applicant Square Footage Owner or Last name First name Authorized agent of owner Corporation or partnership Street ad .
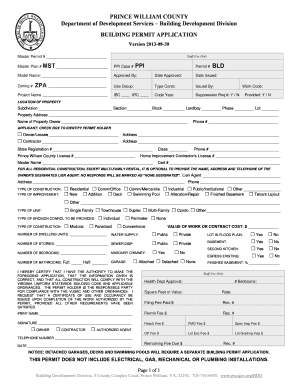
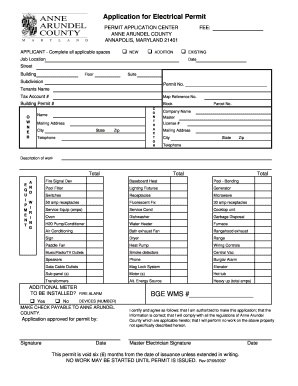
Energy Source Heavy up total amps ADDITIONAL METER TO BE INSTALLED FIRE ALARM DEVICES NUMBER No Yes MAKE CHECK PAYABLE .
be ready to get moreNo pre-authorization is required for outpatient emergency services as well as Post-stabilization Care Services (services that the treating physician views as medically necessary after the emergency medical condition has been stabilized to maintain the patient's stabilized condition) provided in any Emergency Department .
Is Sunshine State Health Medicaid?Sunshine Health enrolls members who are eligible for Medicare and Medicaid. Medicaid includes Full-Benefit Dual Eligible, Qualified Medicare Beneficiary Plus (QMB+) and Specified Low-Income Medicare Beneficiary Plus (SLMB+). Currently, this plan has 2,679 members in 20 counties.
Does Sunshine Health require authorization?Prior approval is required for all services by a provider who is not in the Sunshine Health network. The only exception is for emergency care. Emergency room or urgent care visits do not require prior authorization.
What kind of insurance is Sunshine Health?Sunshine Health is among the largest comprehensive healthcare plans in Florida. We provide quality healthcare coverage with expanded benefits to individuals and families to help them get well and stay well through through our Medicaid, Long Term Care and specialty plans.
Does Florida Medicaid require prior authorization?Prior Authorization Prior approval is required for all services by a provider who is not in the Sunshine Health network. The only exception is for emergency care. Emergency room or urgent care visits do not require prior authorization.
Before prior authorization submission: · STEP ONE: Current insurance plan · STEP TWO: Pharmacy benefit manager (PBM) · STEP THREE: Complete consent form.
Sunshine Health Provider ManualIn addition, some covered services require prior authorization. . documentation of submission of the Medicaid provider registration form Explanation for .
Prior Authorization Forms - AHCCCSThis form provided must be completed monthly, maintained in the member's file at your office, and be available to AHCCCS on request if needed. Contacts. You may .